| [1] |
Tay J, Morris RG, Markus HS. Apathy after stroke:diagnosis,mechanisms,consequences,and treatment[J]. Int J Stroke, 2021, 16(5):510-518.
|
| [2] |
Lopatkiewicz AM, Pera J, Slowik A, et al. Early apathetic,but not depressive,symptoms are associated with poor outcome after stroke[J]. Eur J Neurol, 2021, 28(6):1949-1957.
|
| [3] |
Lammers NA, van Wanrooij LL, van Dalen JW, et al. The course of post-stroke apathy in relation to cognitive functioning:a prospective longitudinal cohort study[J]. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn, 2023, 30(1):94-105.
|
| [4] |
Eurelings LS, van Dalen JW, Ter Riet G, et al. Apathy and depressive symptoms in older people and incident myocardial infarction,stroke,and mortality:a systematic review and meta-analysis of individual participant data[J]. Clin Epidemiol, 2018, 10:363-379.
|
| [5] |
Tang WK, Caeiro L, Lau CG, et al. Apathy and suicide-related ideation 3 months after stroke:a cross-sectional study[J]. BMC Neurol, 2015, 15:60.
|
| [6] |
Zhang HR, Feng YT, Lv HQ, et al. The prevalence of apathy in stroke patients:a systematic review and meta-analysis[J]. J Psychosom Res, 2023, 173:111478.
|
| [7] |
曾宪涛, 刘慧, 陈曦, 等. Meta分析系列之四:观察性研究的质量评价工具[J]. 中国循证心血管医学杂志, 2012, 4(4):297-299.
|
| [8] |
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9):603-605.
|
| [9] |
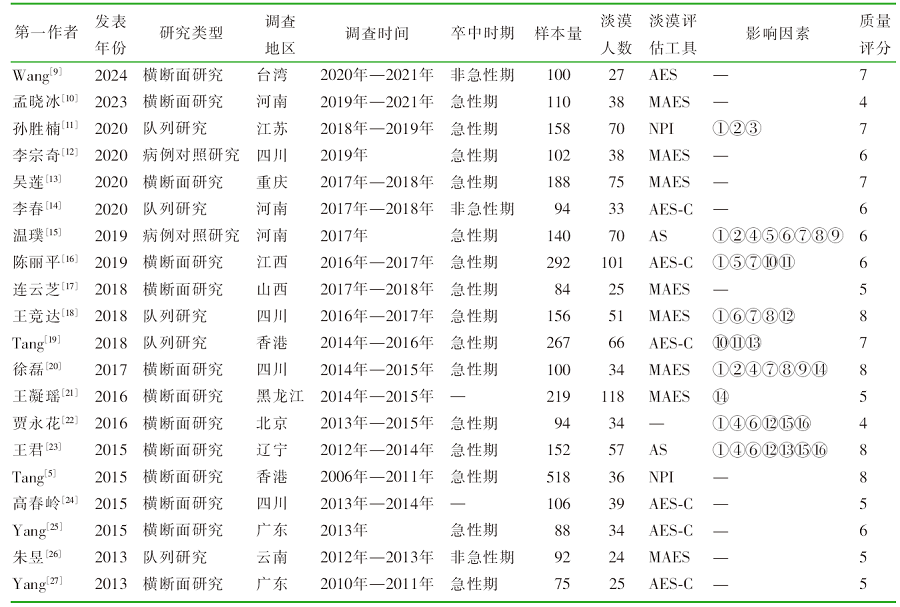
Wang PC, Pai HC. Predictive factors of apathy in stroke survivors during the recovery period[J]. J Neurosci Nurs, 2024, 56(1):25-30.
|
| [10] |
孟晓冰, 李帅帅, 高鹤, 等. 急性脑卒中病人认知功能障碍与情感淡漠及睡眠障碍的相关性[J]. 全科护理, 2023, 21(26):3721-3724.
|
| [11] |
孙胜楠. 急性缺血性脑卒中患者精神行为症状的影响因素及与照料者负担的相关性研究[D]. 大连: 大连医科大学, 2020.
|
| [12] |
李宗奇, 郭晓燕, 胥学梅, 等. 急性缺血性卒中患者睡眠障碍及执行功能障碍与情感淡漠的关系[J]. 中国脑血管病杂志, 2020, 17(12):740-745.
|
| [13] |
吴莲, 何怡, 曹平. 大动脉粥样硬化型脑梗死急性期情感淡漠与血清甲状腺激素水平及卒中功能障碍的相关性[J]. 安徽医药, 2020, 24(5):931-934.
|
| [14] |
李春, 赵高峰, 王新新, 等. 小卒中后情感淡漠发生率的动态变化及对患者生活质量的影响[J]. 中华行为医学与脑科学杂志, 2020, 29(6):511-516.
|
| [15] |
温璞. 缺血性脑卒中患者急性期情感淡漠的影响因素[J]. 中国健康心理学杂志, 2019, 27(2):199-203.
|
| [16] |
陈丽平, 熊思清, 刘怡, 等. 缺血性脑卒中急性期情感淡漠相关影响因素的临床研究[J]. 江西医药, 2019, 54(5):496-499,524.
|
| [17] |
连云芝. 脑梗死急性期淡漠与超敏-C反应蛋白、血尿酸、认知障碍的相关性[J]. 中国实用医刊, 2018, 45(20):17-20.
|
| [18] |
王竞达. 急性缺血性卒中后1年内情感淡漠变化及相关危险因素的前瞻性队列研究[D]. 泸州: 西南医科大学, 2018.
|
| [19] |
Tang WK, Wong LK, Mok VC, et al. Apathy after stroke:potential risk factors and magnetic resonance imaging markers[J]. Hong Kong Med J, 2018, 24(3):18-20.
|
| [20] |
徐磊, 喻明, 谭华. 缺血性卒中急性期情感淡漠的发生率及相关因素分析[J]. 天津医药, 2017, 45(3):301-305.
|
| [21] |
王凝瑶, 孙伟. 卒中后淡漠相关因素的临床研究[J]. 中国医药科学, 2016, 6(6):143-145.
|
| [22] |
贾永花, 杜会山. 缺血性卒中患者急性期淡漠情绪障碍的影响因素研究[J]. 实用心脑肺血管病杂志, 2016, 24(7):32-35.
|
| [23] |
王君, 于治华, 王正则, 等. 脑梗死急性期淡漠预测因素的研究[J]. 中国康复理论与实践, 2015, 21(8):934-938.
|
| [24] |
高春岭. 无症状性脑梗死患者情感淡漠及相关性因素研究[D]. 泸州: 四川医科大学, 2015.
|
| [25] |
Yang S, Hua P, Shang X, et al. Deficiency of brain structural sub-network underlying post-ischaemic stroke apathy[J]. Eur J Neurol, 2015, 22(2):341-347.
|
| [26] |
朱昱. 脑梗死患者的情感淡漠及其与认知障碍和抑郁的关系[D]. 昆明: 昆明医科大学, 2013.
|
| [27] |
Yang SR, Hua P, Shang XY, et al. Predictors of early post ischemic stroke apathy and depression:a cross-sectional study[J]. BMC Psychiatry, 2013, 13:164.
|
| [28] |
Caeiro L, Ferro JM, Costa J. Apathy secondary to stroke:a systematic review and meta-analysis[J]. Cerebrovasc Dis, 2013, 35(1):23-39.
|
| [29] |
van Dalen JW, et al. Moll van Charante EP,Nederkoorn PJ, Poststroke apathy[J]. Stroke, 2013, 44(3):851-860.
|
| [30] |
Sagen-Vik U, Finset A, Moum T, et al. The longitudinal course of anxiety,depression and apathy through two years after stroke[J]. J Psychosom Res, 2022, 162:111016.
|
| [31] |
Marquez-Ortiz RA, Tesic V, Hernandez DR, et al. Neuroimmune support of neuronal regeneration and neuroplasticity following cerebral ischemia in juvenile mice[J]. Brain Sci, 2023, 13(9):1337.
|
| [32] |
Moretti R, Signori R. Neural correlates for apathy:frontal-pre-frontal and parietal cortical- subcortical circuits[J]. Front Aging Neurosci, 2016, 8:289.
|
| [33] |
Gerstenecker A, Duff K, Mast B, et al. Behavioral abnormalities in progressive supranuclear palsy[J]. Psychiatry Res, 2013, 210(3):1205-1210.
|
| [34] |
Theis H, Prange S, Bischof GN, et al. Impulsive-compulsive be-haviour in early Parkinson’s disease is determined by apathy and dopamine receptor D3 polymorphism[J]. NPJ Parkinsons Dis, 2023, 9(1):154.
|
| [35] |
Tang WK, Chen YK, Liang HJ, et al. Location of infarcts and apathy in ischemic stroke[J]. Cerebrovasc Dis, 2013, 35(6):566-571.
|
| [36] |
Onoda K, Kuroda Y, Yamamoto Y, et al. Post-stroke apathy and hypoperfusion in basal Ganglia:SPECT study[J]. Cerebrovasc Dis, 2011, 31(1):6-11.
|
| [37] |
Carnes-Vendrell A, Deus J, Molina-Seguin J, et al. Depression and apathy after transient ischemic attack or minor stroke:prevalence,evolution and predictors[J]. Sci Rep, 2019, 9(1):16248.
|
| [38] |
Douven E, Staals J, Schievink SHJ, et al. Personality traits and course of symptoms of depression and apathy after stroke:results of the CASPER study[J]. J Psychosom Res, 2018, 111:69-75.
|
| [39] |
van Almenkerk S, Smalbrugge M, Depla MF, et al. Apathy among institutionalized stroke patients:prevalence and clinical correlates[J]. Am J Geriatr Psychiatry, 2015, 23(2):180-188.
|
| [40] |
Le Heron C, Plant O, Manohar S, et al. Distinct effects of apathy and dopamine on effort-based decision-making in Parkinson’s disease[J]. Brain, 2018, 141(5):1455-1469.
|
| [41] |
Padala PR, Desouza CV, Almeida S, et al. The impact of apathy on glycemic control in diabetes:a cross-sectional study[J]. Diabetes Res Clin Pract, 2008, 79(1):37-41.
|